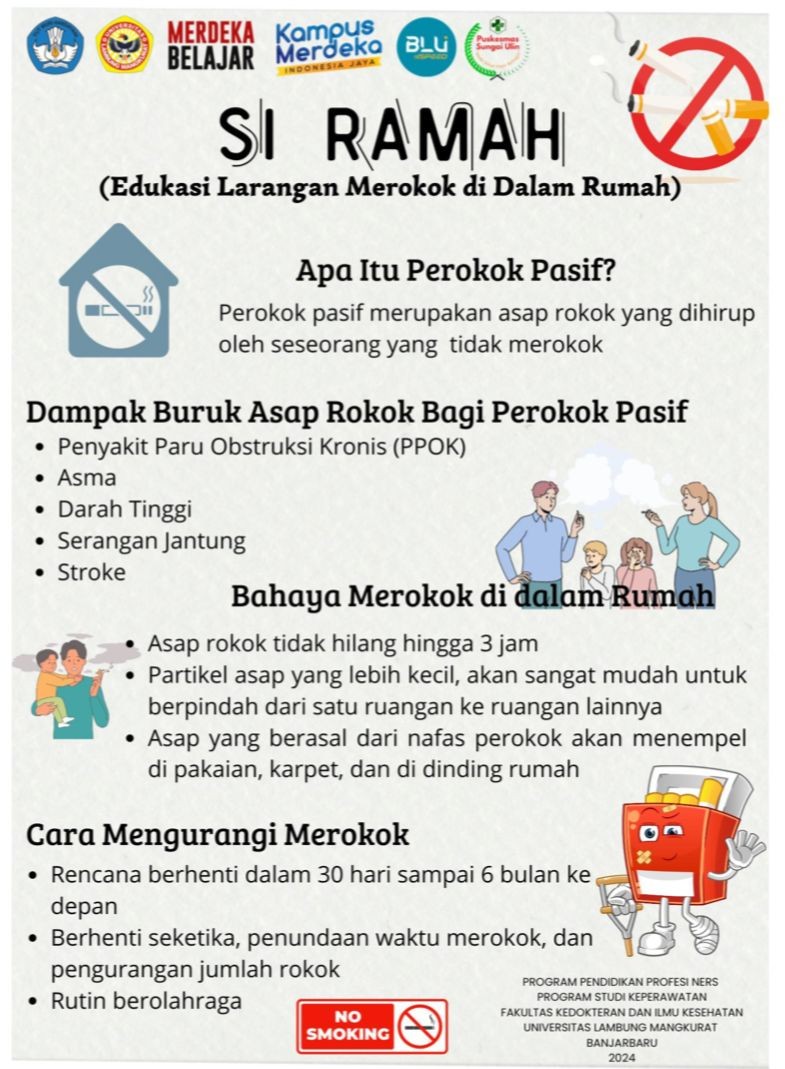
Edukasi Kesehatan dan Testimoni Penyintas sebagai Strategi Penguatan Komitmen Keluarga terhadap Larangan Merokok di Dalam Rumah
Health Education and Survivor Testimonies as a Strategy to Strengthen Family Commitment to No Smoking Policy at Home
DOI:
https://doi.org/10.64621/hjics.v1i2.48Keywords:
edukasi, keluarga, merokok, penyintas, rumah tanggaAbstract
Latar belakang: Paparan asap rokok dalam rumah tangga masih menjadi isu serius dalam kesehatan masyarakat. Merokok di dalam rumah merupakan salah satu faktor risiko utama paparan asap rokok pasif yang berdampak negatif pada kesehatan anggota keluarga, terutama anak-anak dan lansia. Penguatan komitmen keluarga terhadap larangan merokok di dalam rumah menjadi langkah penting dalam mengurangi risiko tersebut.Kegiatan pengabdian ini bertujuan meningkatkan pemahaman dan kesadaran keluarga, khususnya dengan anggota penyintas penyakit akibat rokok, mengenai dampak merokok di dalam rumah. Metode: Program dilaksanakan dalam bentuk penyuluhan dan sesi berbagi pengalaman oleh penyintas. Pengukuran dilakukan menggunakan pre-post test dan observasi partisipatif. Hasil: Peserta mengalami peningkatan pemahaman sebesar 32% pasca kegiatan, serta tumbuhnya komitmen untuk menciptakan rumah bebas rokok. Kesimpulan: Program SI RAMAH menunjukkan efektivitas pendekatan berbasis pengalaman sebagai edukasi kesehatan komunitas. Program ini direkomendasikan untuk diadopsi secara luas sebagai model penguatan komitmen keluarga dalam pencegahan paparan asap rokok.
Downloads
References
Abraham, C., & Sheeran, P. (2014). The health belief model. Cambridge Handbook of Psychology, Health and Medicine, Second Edition, January, 97–102. https://doi.org/10.1017/CBO9780511543579.022
Baishya, M. L., Collins, B. N., & Lepore, S. J. (2022). Antecedents of Self-Efficacy to Achieve Smoking-Behavior-Change Goals among Low-Income Parents Enrolled in an Evidence-Based Tobacco Intervention. International Journal of Environmental Research and Public Health, 19(20). https://doi.org/10.3390/ijerph192013573
Behbod B, S. M. B. R. R. R., & Webster, P. (2018). Family and carer smoking control programmes for reducing children’s exposure to environmental tobacco smoke. Cochrane Database of Systematic Reviews, 1. https://doi.org/10.1002/14651858.CD001746.pub4
Berman, T., Rorman, E., Groisman, L., Keinan-Boker, L., Shimony, T., & Barnett-Itzhaki, Z. (2023). Association between parental smoking and child exposure to environmental tobacco smoke in Israel. Israel Journal of Health Policy Research, 12(1), 37. https://doi.org/10.1186/s13584-023-00585-6
Dai, S., Au, C. T., Chan, M. H. M., Kam, R. K. T., Li, A. M., & Chan, K. C.-C. (2021). Parental Knowledge, Attitude, and Practice on Tobacco Use, Smoking Cessation, and Children’s Environmental Tobacco Smoke Exposure. Frontiers in Public Health, 9, 733667. https://doi.org/10.3389/fpubh.2021.733667
GATS. (2021). GATS | GLOBAL ADULT TOBACCO SURVEY Indonesia 2021.
Hanafin, J., Sunday, S., & Clancy, L. (2021). Friends and family matter Most: a trend analysis of increasing e-cigarette use among Irish teenagers and socio-demographic, personal, peer and familial associations. BMC Public Health, 21(1), 1988. https://doi.org/10.1186/s12889-021-12113-9
Jenssen, B. P., Kelly, M. K., Faerber, J. A., Asch, D. A., Shults, J., Schnoll, R. A., & Fiks, A. G. (2023). Pediatrician-Delivered Smoking-Cessation Messages for Parents: An Update. Academic Pediatrics, 23(6), 1140–1141. https://doi.org/10.1016/j.acap.2023.05.008
Lafont, M., Morin, C., Arrouy, A., Rabeau, A., Labouret, G., Roditis, L., Michelet, M., & Mittaine, M. (2021). Pediatrician intervention impacts parental smoking in cystic fibrosis, diabetes, and bronchiolitis. Pediatric Pulmonology, 56(6), 1716–1723. https://doi.org/10.1002/ppul.25277
Liu, D., Ren, Y., Wu, T., Shen, H., Yan, P., Meng, Y., Zhang, Q., Zhang, J., Bai, P., & Zhao, J. (2022). Parental smoking exposure before and during pregnancy and offspring attention-deficit/hyperactivity disorder risk: A Chinese child and adolescent cohort study. Frontiers in Public Health, 10, 1017046. https://doi.org/10.3389/fpubh.2022.1017046
Loukili, H., Fatimy, R. El, & Amine, M. (2024). Self-efficacy and health warnings as predictors of smoking cessation intent among Moroccan adolescents: Evidence from the Global Youth Tobacco Survey data. Tobacco Induced Diseases, 22. https://doi.org/10.18332/tid/185647
Nabi-Burza, E., Drehmer, J. E., Walters, B. H., Willemsen, M. C., Zeegers, M. P. A., & Winickoff, J. P. (2021). Smoking Cessation Treatment for Parents Who Dual Use E-Cigarettes and Traditional Cigarettes. Journal of Smoking Cessation, 2021, 6639731. https://doi.org/10.1155/2021/6639731
Nabi-Burza, E., Wasserman, R., Drehmer, J. E., Walters, B. H., Luo, M., Ossip, D., & Winickoff, J. P. (2021). Spontaneous Smoking Cessation in Parents. Journal of Smoking Cessation, 2021, 5526715. https://doi.org/10.1155/2021/5526715
Notley, C., Brown, T. J., Bauld, L., Boyle, E. M., Clarke, P., Hardeman, W., Holland, R., Hubbard, M., Naughton, F., Nichols, A., Orton, S., Ussher, M., & Ward, E. (2022). Development of a Smoke-Free Home Intervention for Families of Babies Admitted to Neonatal Intensive Care. International Journal of Environmental Research and Public Health, 19(6). https://doi.org/10.3390/ijerph19063670
Scheffers-van Schayck, T., Mujcic, A., Otten, R., Engels, R., & Kleinjan, M. (2021). The Effectiveness of Smoking Cessation Interventions Tailored to Smoking Parents of Children Aged 0-18 Years: A Meta-Analysis. European Addiction Research, 27(4), 278–293. https://doi.org/10.1159/000511145
Stanhope, M., & Lancaster, J. (2014). Foundations of Nursing in the Community: Community-Oriented Practice (4th ed.). Elsevier Mosby.
Visser, J. E. M., Rozema, A. D., Kunst, A. E., & Kuipers, M. A. G. (2024). Smoking Cessation Support in Social and Community Service Organizations: Potential Activities, Barriers, and Facilitators. Nicotine & Tobacco Research : Official Journal of the Society for Research on Nicotine and Tobacco, 26(7), 922–930. https://doi.org/10.1093/ntr/ntae004
Williams, B. S., Smith, S. S., Marbin, J. N., Huang, M. Z., Garell, C. L., Kosack, A. S., Shaikh, U., Tebb, K. P., & Fiore, M. C. (2021). Addressing Environmental Smoke Exposure During Pediatric Hospitalization: Attitudes and Practices of Pediatric Nurses Versus Respiratory Therapists. Respiratory Care, 66(2), 275–280. https://doi.org/10.4187/respcare.08038
World Health Organization. (2023). Tobacco.
Žarković, M., Sommer, G., Nigg, C., Sláma, T., Schneider, C., Ansari, M., von der Weid, N., Schindera, C., & Kuehni, C. E. (2024). Parental smoking and respiratory outcomes in young childhood cancer survivors. Pediatric Blood & Cancer, 71(11), e31310. https://doi.org/10.1002/pbc.31310
Downloads
Published
Issue
Section
License
Copyright (c) 2025 Yulia Yunara, Annisa Febriana, Fajar Az-zahrawi, Annisa Ulfah Febrianty (Author)

This work is licensed under a Creative Commons Attribution 4.0 International License.